The pandemic has accelerated telehealth care adoption in the last three years, with more patients and providers utilizing these virtual care services. They allow patients to consult healthcare professionals remotely, using technology convenience. This article will explain what telehealth is, its history and evolution, the types of telemedicine, and the advantages it offers patients and providers. We’ll also explore the technologies powering telemedicine, how it is applied in practice, regulatory considerations, challenges, and the future of virtual care.
Table of Contents
Understanding Telehealth Care
Definition
Telemedicine means exchanging medical information from one location to another using electronic communications technology. It allows patients to access healthcare services remotely through video conferencing, phone calls, mobile apps, and other digital devices. Unlike traditional in-person appointments, it provides care virtually.
History of Telehealth
Technologies that deliver remote healthcare dates back to the 1960s when clinicians used video conferencing to provide consultations. NASA also used Telehealth to monitor astronauts’ health in space during this decade. However, high costs limited widespread adoption until the 2000s, when telemedicine saw a resurgence due to technological advancements and internet connectivity.
In the 2010s, telehealth increased with the proliferation of high-speed internet, smartphones, tablets, and mobile medical devices. The COVID-19 pandemic further accelerated the uptake of Telehealth globally. Patients and providers adopted virtual care solutions to continue offering healthcare services safely. During the pandemic, regulatory barriers were relaxed, reimbursement policies expanded, and telemedicine became mainstream.
Types of accessible Offers
There are three primary modalities:
- Real-time video conferencing: Synchronous virtual care involves a live video interaction between the patient and provider. It simulates an in-person visit.
- Store-and-forward: Patients share their medical data, like lab reports and images, to providers electronically for evaluation. This asynchronous form of virtual care does not require real-time interaction.
- Remote patient monitoring: Devices are used to collect health data from patients in one location and transmit it electronically to providers in a different area for assessment. Examples include home blood pressure monitors and wearable heart rate trackers.
Advantages of Virtual Healthcare
Accessibility and Convenience
One significant benefit of telemedicine is the improved access to healthcare for patients, especially those restricted by geography, mobility issues, or busy schedules. Patients in remote areas can consult doctors in significant hospitals virtually, while those with chronic conditions can avoid unnecessary visits by connecting online. Appointment availability with telehealth urgent care and Virtual Care also provides more flexibility.
Cost Savings
Both providers and patients benefit from reduced expenses. Virtual visits cost less than in-person appointments since they don’t incur overhead charges associated with operating physical clinics. Patients save money on travel and wait times. Providers can also reach more patients in less time, improving productivity.
Time Efficiency
With telemedicine, patients skip the travel and waiting time associated with in-person consultations. Appointments can be scheduled quickly through telehealth platforms. The overall care journey is streamlined, saving time for both patient and physician.
Improved Continuity of Care
Easy access to patient medical records and history enables providers to coordinate care and collaborate more efficiently via telemedicine. Sharing health data between primary care doctors and specialists is streamlined, ensuring continuity of care.

Common Technologies Used
Telehealth Platforms
These services leverage many technologies, including telehealth platforms that enable video visits, patient portals, remote monitoring devices, and smartphone apps. Providers use HIPAA-compliant software to conduct secure virtual consultations, document visits, prescribe medications, and share medical records. Major Virtual Care providers include Teladoc Health, Doctor on Demand, and American Well.
Security and Privacy
Data privacy and security is a top concern for providers. Providers adhere to cybersecurity best practices and HIPAA guidelines to protect patient information. Data encryption, firewalls, authentication, and stringent access controls protect telehealth systems and data.
Telehealth Devices
Digital Health devices include smartphones, computers, and medical peripherals such as wearables into their ecosystem. Patients use these devices to share health information with providers. High-definition (HD) cameras and built-in scopes allow for remote evaluations. Bluetooth-enabled devices monitor vital signs such as blood pressure and glucose levels sent to providers. Integrating Internet of Things (IoT) networks will lead to more advanced remote monitoring.
Telemedicine in Practice
Telehealthcare as Primary Care solution
Many primary care providers now integrate telehealth platforms from providers like GoodRx Telehealth and Amazon Clinic to offer patients virtual and in-person service options. Online appointments for routine care, like prescription refills, lab follow-ups, minor illnesses, mental health counseling, etc., reduce unnecessary office visits while improving continuity of care.
Specialty Care and Telehealth Care
Specialists like cardiologists, neurologists, and psychiatrists increasingly rely on telemedicine for follow-up visits, medication management, chronic disease management, and telemonitoring—technologies like store-and-forward and remote patient monitoring support specialized care.
Remote Monitoring
Wearable devices and at-home medical equipment facilitate continuous remote monitoring for chronic conditions and post-operative recovery. Doctors can identify complications early and initiate treatment quickly, preventing unnecessary ER visits and hospital readmissions. Those practices are transforming areas like intensive care, cardiology, and cancer care.
Legal and Regulatory Considerations
Licensing and Credentialing
For telemedicine services, providers must be licensed and credentialed in the state where the patient is located. Interstate compacts allowing telehealth providers to serve patients across state lines are simplifying licensing requirements.
Telemedicine Regulations
Telemedicine is regulated through a patchwork of state and federal policies related to reimbursement, prescribing practices, and physician licensing. While states are gradually updating telehealth policies, advocacy groups like the American Telehealth Association are pushing for more uniform national telehealth regulations.
The Challenges and Solutions
The Digital Divide
Limited access to broadband internet and lack of familiarity with technology prevent telemedicine adoption among marginalized communities. Targeted government programs can help close this telehealth gap through digital literacy initiatives, device/internet assistance, and improved rural connectivity.
Technological Barriers
Privacy and data security risks, integration challenges with legacy healthcare IT systems, and gaps in interoperability are some technology obstacles affecting telemedicine. Upgrading cyber defenses, modernizing health IT infrastructure, and promoting open API standards would help overcome these barriers.
Patient Engagement
Encouraging patients to participate in telemedicine instead of passively receiving care is critical for improved health outcomes. Strategies like care reminders, virtual waiting rooms, two-way communication, and patient education around telehealth strengthen engagement.
The Future of Virtual Care
Technological Advancements
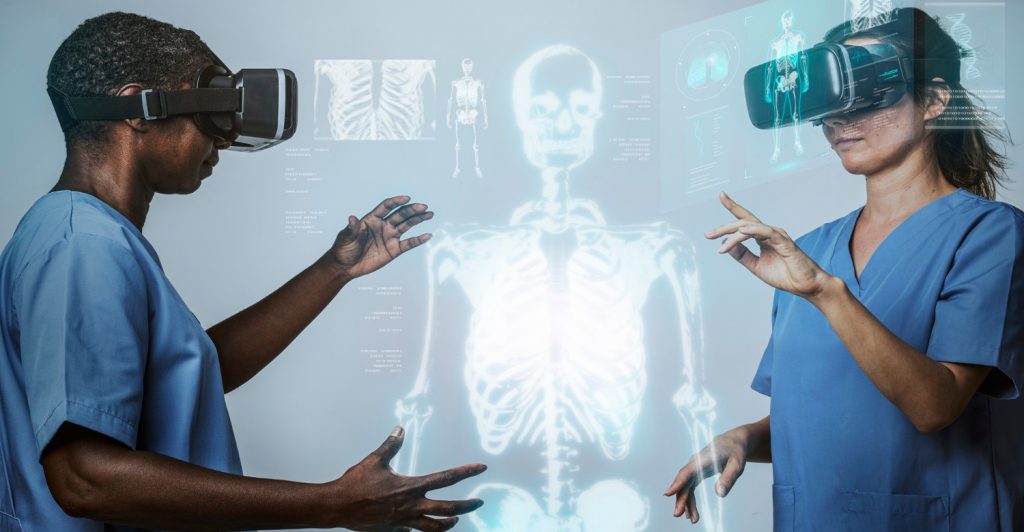
Advances in augmented reality, haptics, AI, 5G, and the Internet of Medical Things will make telemedicine more innovative, immersive, and seamless. Telehealth will extend beyond video visits to become an always-on care channel integrated with in-person and digital health services.
Telemedicine’s Role in Healthcare
Virtual Care will become a core component of regular healthcare delivery. It will complement in-person services while making care more proactive, accessible, and efficient. Telehealth’s ability to transcend geographic barriers supports population health goals like epidemic preparedness and equal access.
Conclusion and Key Takeaways
Telehealthcare has transformed from a niche innovation to a vital digital health channel connecting patients and clinicians. Its advantages, like increased access, convenience, and lower costs, are clear. However, challenges around technological barriers, regulations, and patient engagement remain. As telehealth platforms, devices, and networks become more advanced, secure, and integrated, the scope of virtual care will continue expanding. Virtual Care is undoubtedly revolutionizing healthcare accessibility and delivery models for the future.
FAQs
Q1: What is telemedicine?
A1: It is the remote delivery of healthcare services through telecommunications technology. Patients can consult healthcare providers virtually instead of traditional in-person visits.
Q2: How does a telehealth visit work?
A2: It typically involves a video call between the patient and the healthcare provider through a telehealth platform. The provider can assess the patient, diagnose conditions, prescribe medications, and follow up on ongoing treatments – all virtually.
Q3: When should you use telehealth?
A3: It is appropriate for routine consultations like medication refills, lab follow-ups, chronic condition management, mental health counseling, and minor illnesses that a primary care provider can evaluate virtually. It should not replace emergency care.
Q4: Does health insurance cover telemedicine?
A4: Many major health plans now cover Virtual Care services, especially following temporary expansions of telehealth coverage during the COVID-19 pandemic. Verify your plan’s telemedicine benefits specifically before your visit. Medicare and Medicaid also cover certain telehealth services.
Q5: What kind of care can you get via telehealth care?
A5: Primary care, mental health counseling, dermatology, and chronic disease management are the most common services. However, an increasingly wide range of specialties, from cardiology to physiotherapy, now offer virtual visits.




